Researchers have discovered that some immunotherapy treatments used to treat cancer can cause fertility damage.
It means these treatments could affect the future fertility and hormonal health of female cancer survivors, prompting experts to call for more research and preventative measures, such as freezing eggs.
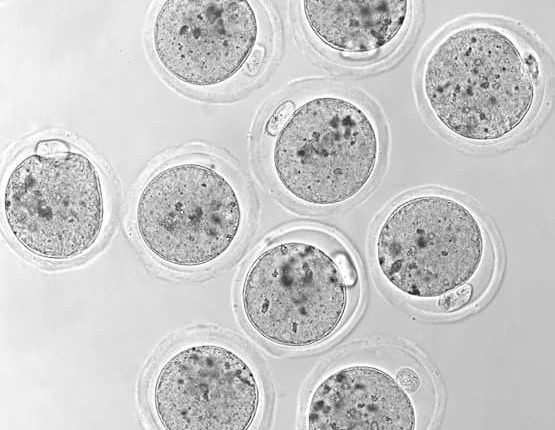
Led by the Biomedicine Discovery Institute at Monash University and the Peter MacCallum Cancer Centre, the pre-clinical trial showed that immune checkpoint inhibitors, a common type of immunotherapy drug, resulted in permanent damage to mouse ovaries and the eggs stored inside.
Traditional cancer therapies, such as chemotherapy and radiotherapy, are already linked to permanent, negative side effects on the ovaries. This can lead to infertility and premature menopause in young girls and women.
Published in Nature Cancer, researchers found that checkpoint inhibitor immunotherapy reduced
the number and quality of their eggs, interfered with ovulation, and disrupted the fertility cycle.
Until now the potential fertility side effects of immunotherapy, an emerging and increasingly common cancer treatment that stimulates the immune system, have been unknown.
The study found that a type of immunotherapy called immune checkpoint inhibitors, which ‘release the brakes’ on the immune system to enhance a patient’s ability to fight cancer, could impair immediate and future fertility.
Its authors said studies in female patients were now needed to investigate the findings. In the meantime, fertility preservation through egg or embryo freezing should be considered for women using these immunotherapies.
Co-lead author Lauren Alesi, a PhD candidate in the Monash Biomedicine Discovery Institute Ovarian Biology Laboratory, said human studies must now be prioritised.
“Initially these treatments were thought to be less damaging (than chemo and radiotherapy) in the context of off-target effects to the body in general,” Ms Alesi said. “However, it is now clear that inflammatory side effects in other organ systems are quite common with these drugs.
“Our study highlights that caution should be exercised by clinicians and their patients, for whom fertility may be a concern. Studies in women receiving these drugs must now be prioritised.”
Peter MacCallum Cancer Centre Specialist Medical Oncologist Professor in breast cancer and a senior author on the study Sherene Loi said further research into how these drugs impact the ovarian function and fertility of women receiving these drugs must be prioritised and should be included in future clinical trials involving women of reproductive age.
“Our study further highlights that fertility discussions are critical for all age appropriate women who are recommended to receive chemotherapy as well as immunotherapy,” Professor Loi said.
“Appropriate interventions that can preserve fertility and ovarian function can be implemented to facilitate pregnancies in the future, post completion of treatment. These interventions need to be implemented in a timely manner, so as not to delay anti-cancer treatment.
“Immunotherapy is now becoming a standard of care for many women with curable early stage breast cancer, due to impressive results in reducing breast cancer recurrences, but further research into the long-term effects of immunotherapy is needed.”
Apart from drugs that block ovaries from producing hormones during chemotherapy, and strategies to prevent premature menopause in younger women, Ms Alesi said egg and embryo freezing was the only fertility preservation measure available.
She said it was important to remember that embryo freezing was expensive, invasive and did not prevent ovarian damage. This meant that premature menopause could still be a risk for these women.
“Therefore, we are now prioritising investigation of targeted ovarian preservation strategies that aim to prevent the damage to the ovary from occurring in the first place, without interfering with the drugs’ ability to fight the cancer” she said.
Ms Alesi said other immunotherapy classes also need to be assessed.
“Our results may have implications for other immunotherapies, since our results have revealed a close relationship between immune cells, the communication molecules (cytokines) they release, and regulating many aspects of fertility,” she said.
Read the full paper published in Nature Cancer, titled Checkpoint inhibitor immunotherapy diminishes oocyte number and quality in mice: https://www.nature.com/articles/s43018-022-00413-x
DOI: 10.1038/s43018-022-00413-x
About the Monash Biomedicine Discovery Institute at Monash UniversityCommitted to making the discoveries that will relieve the future burden of disease, the Monash Biomedicine Discovery Institute at Monash University brings together more than 120 internationally-renowned research teams. Spanning seven discovery programs across Cancer, Cardiovascular Disease, Development and Stem Cells, Infection, Immunity, Metabolism, Diabetes and Obesity, and Neuroscience, Monash BDI is one of the largest biomedical research institutes in Australia. Our researchers are supported by world-class technology and infrastructure, and partner with industry, clinicians and researchers internationally to enhance lives through discovery.
About Peter Mac
Peter MacCallum Cancer Centre is a world-leading cancer research, education and treatment centre and Australia’s only public health service solely dedicated to caring for people affected by cancer.
Comments are closed.